Danger of New Cholesterol Lowering Drugs
Statins don’t always lower high cholesterol levels enough. New PCSK9 inhibitors can help. But you need to know about a danger of new cholesterol lowering drugs.
When you think of cholesterol lowering drugs, statins likely come to mind. But they don’t work for everyone. There are other drugs that can be added to statins to reduce LDL (low density lipoprotein, also called “bad” cholesterol) but they aren’t always successful, either.
However, a newer class of medications, proprotein convertase subtilisin/kexin type 9 ― PCSK9 inhibitors, for short ― have been shown to be remarkably successful in dramatically lowering harmful LDL in people who don’t have success with statins and who are at the highest risk for a cardiovascular event.
But a danger of new cholesterol drugs in this class of medications has been documented, and it can be life-threatening. However, if you assume that means PCSK9s have some newly discovered harmful side-effects, think again.
Surprisingly, the danger of the new cholesterol lowering drugs in this class is their cost. The result is too many people with extremely high cholesterol levels are not filling their prescriptions because of the cost, causing the risk of heart attacks and stroke to skyrocket in people who need PCSK9s the most.
YOU MIGHT ALSO LIKE: Symptoms of High Cholesterol
PCSK9s can save lives — if you take them
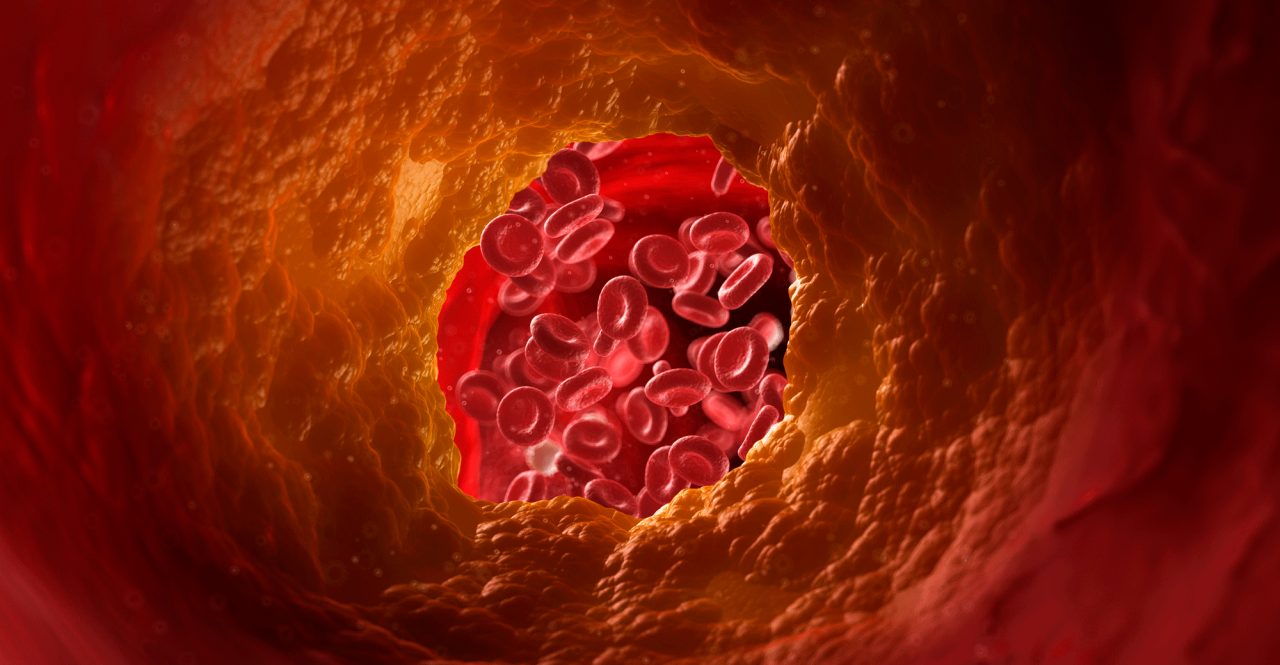
Too high LDL is a well-known risk factor for cardiovascular disease. Over time it can result in artery-clogging plaque and trigger heart attacks and stroke. Although many people can lower LDL with exercise and weight loss, others need medications and, since the late l980s, statins have been the drug of choice as first-line treatment for elevated cholesterol.
But for those with either familial hypercholesterolemia (FH) or clinical atherosclerotic cardiovascular disease (ASCVD) on maximally tolerated statin therapy who still have extremely high LDL levels, the 2015 Food and Drug Administration approval of PCSK9 inhibitors was a potential life-saving development.
For example, people with FH, a not uncommon inherited genetic defect, are born with higher than normal LDL that continues to get higher over time. The result is a five times higher risk for coronary heart disease over a 30-year span if their cholesterol is not adequately reduced, according to the American Heart Association (AHA).
Half of men with untreated FH have a heart attack or angina before they turn 50, some even having cardiac events in their 20s. Meanwhile, 30 percent of untreated women with FH experience a heart attack before they turn 60. But PCSK9s have, finally, provided a successful treatment to reduce these risks.
PCSK9 inhibitors work differently than statins. They are monoclonal antibodies, designed to target and inactivate a specific protein in the liver (convertase subtilisin kexin 9), which substantially lowers the amount of LDL circulating in the bloodstream. The medication is not in pill form but is self-administered under the skin with a pen device once or twice a month.
The potentially life-threatening danger of new cholesterol lowering drugs in the PCSK9 inhibitor class is their expense. The medications don’t work if people don’t take them, and large numbers can’t take them — or refuse to — because prescriptions for the medication are not accepted by all insurance plans or often require co-pays of hundreds of dollars.
Heart attack risk soars without needed PCSK9s
People with FH or ASCVD who don’t obtain their prescribed PCSK9 inhibitors experience more heart attacks, strokes, and other cardiovascular events, according to a study published in Circulation: Cardiovascular Quality and Outcomes. In fact, FH Foundation researchers found an immediate 16 percent increased risk of a cardiovascular events over the course of 12 months without PCSK9 prescription therapy.
In order to analyze whether unfilled and rejected PCSK9 inhibitor prescriptions had a direct impact on heart attacks, strokes, and other cardiac problems, data was collected from 139,036 patients with high cholesterol over the age of 18 between August 2015 and December 2017. The findings showed people needing PCSK9s whose prescription claims were rejected by insurance, or whose prescription was approved but not filled (usually because of a high co-pay the patient could not afford). had an immediate 21 percent increased risk of a cardiovascular event.
Although people with FH had the highest risk of heart attack, 63 percent of their prescriptions were rejected by insurance.
"While we know that someone who has had a heart attack or other cardiovascular event is much more likely to have a second event and is at much higher risk than the general population, this new finding underscores that individuals with FH are at as high a risk. It is imperative that we initiate comprehensive treatment early in life, and that individuals receive the medications they have been prescribed," said researcher Daniel J. Rader, MD, chairman of the department of Genetics in the Perelman School of Medicine at the University of Pennsylvania and chief scientific advisor of the FH Foundation.
Don’t abandon treatment or hope
There’s no doubt PCSK9 inhibitors are expensive. At the time the FH research was conducted, the prescription treatment cost about $14,000 a year, the AHA points out. For those whose insurance did cover the medication, the average copayment for prescriptions people failed to fill was $233.30 — more than $100 higher than other prescription drugs.
But if you need a PCSK9 inhibitor and can’t afford the medication, don’t give up. Contact your doctor ASAP and see if increasing statins or other medications may help. And ask your health provider to contact your insurance company if your prescription has been denied, to explain why you need this medication.
The good news is the AHA and other medical experts are working to make these important cholesterol-lowering drugs more accessible to those in need.
"Following a thorough review of the science, the American Heart Association guidelines now support the use of PCSK9 inhibitors for certain populations - after use of statins and ezetimibe — and we encourage clinicians and payors to take this into consideration in determining prescription approvals," said Donald Lloyd-Jones, MD, chairman of the department of preventive medicine at Northwestern University and a member of the writing committee for the American Heart Association's 2018 cholesterol guidelines.
"Additionally, the Association has taken bold action in working directly with pharmaceutical companies to address the considerable costs that can hinder access to life-saving medications. So, we hope to see this trend turning and for future data to show that people have access to the medications they need and are using them to their greatest benefit."
Updated:
November 27, 2019
Reviewed By:
Janet O’Dell