Colon (Colorectal) Cancer Diagnosis
A colon cancer diagnosis requires a colonoscopy and lab tests of tissue samples taken from your colon. The earlier you have the procedure, the better your prognosis.
How is colorectal cancer diagnosed?
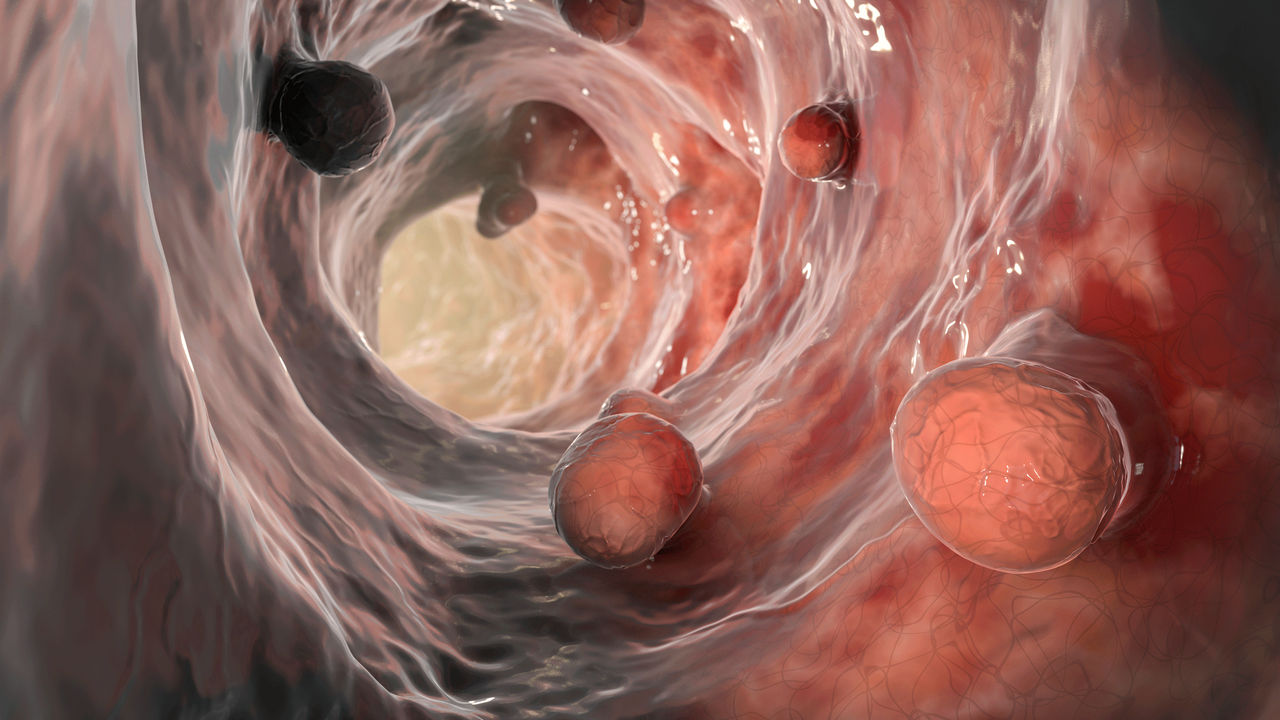
Colorectal cancer is cancer of the colon or the rectum. The colon refers to the first five feet of your large intestine; the rectum is the last six inches.
You may first hear you may have colorectal cancer if blood appears in a mail-in sample of feces from at home test, or if your gastroenterologist discovers precancerous or cancerous growths, called polyps, during a colonoscopy.
You should not ignore the danger signs of colon cancer, in particular blood in your stool, which can make it look black, or blood leaking from your rectum.
Other possible symptoms include:
- Unexplained abdominal cramps or pain that lasts more than a few days
- A persistent urge for a bowel movement after you have had one
- Unexplained weakness
- Fatigue
- Unintended weight loss
- Anemia
Although those symptoms could have many other causes, often inflammatory bowel disease, your doctors need to evaluate them, especially if you have not had a recent colonoscopy.
YOU MIGHT ALSO LIKE: How Colon Cancer Starts
Am I too young for colorectal cancer?
You should begin colon cancer screening at age 45. But more young people are being diagnosed in their 20s and 30s, usually at a more dangerous, advanced stage.
People who have a higher risk for colon cancer are of African American heritage or have a family history of the cancer. They should consider screening earlier.
It’s also important to know that 70 percent of colorectal cancers occur in people with no obvious risk factors, including a family history of colon cancer.
What are the risk factors for colorectal cancer?
The older you are, the more likely you are to develop colon cancer. Most cases occur after the age of 50.
Up to 10 percent of cases can be traced to genes from your parents, so tell your doctor if a parent had any kind of cancer, Lynch syndrome, or familial adenomatous polyposis.
Cigarette smokers are 40 percent more likely to die of colorectal cancer. Other colon cancer risk factors include:
- Drinking too much alcohol
- A lack of exercise
- Extra fat around the waist
- A diet high in red, processed, or charred meats
You are also at more risk if you have type 2 diabetes or inflammatory bowel disease.
What is a biopsy?
During a colonoscopy, you may receive mild sedation.
If your gastroenterologist finds polyps during a colonoscopy, he or she will remove sample tissue and send it to a lab to be examined under a microscope for cancer cells. It may be a few days before you hear your results. The process, called a biopsy, is the only sure way to diagnose colorectal cancer.
To diagnose the cause of diarrhea or belly pain, you might have a sigmoidoscopy, which allows your doctor to see the first third of your colon, near your rectum and anus. The test doesn’t require sedation.
Both colonoscopy and sigmoidoscopy require inserting a tube with a small video camera on the end and removing samples of any polyps.
You may need a surgical biopsy if a large or hard-to-reach polyp is discovered. You'll receive general anesthesia so you fall asleep and don't feel the procedure. You may also have to stay overnight in the hospital. It may take a few days before you can return to your normal routine.
Most polyps are benign (not cancerous). You might have a dysplastic polyp, which shows abnormal cell growth but is not yet cancerous. Dysplastic polyps raise your risk of developing more polyps and cancer.
Getting your test results
When your healthcare provider has the results of your biopsy, he or she will contact you. Your provider will talk with you about other tests you may need if colorectal cancer is found. Make sure you understand the results and what follow-up tests you need.
You may need blood tests and various scans to evaluate any cancerous growth. Your doctors will try to determine the stage of your cancer, which is based on its size and how far it has spread.
The stages of colorectal cancer
Knowing the stage of your cancer helps you anticipate how much treatment you will need.
- Stage 0: Abnormal cells in the wall, called the mucosa, of your colon, which can be removed during a colonoscopy.
- Stage I: Abnormal cells in the mucosa and submucosa, which lies immediately underneath the wall of your colon, and possibly a layer of muscle. You may need surgery.
- Stage II: Abnormal cells that have spread past your colon wall. In the most serious kind, Stage IIc, they have spread past your colon. You will need surgery and possibly chemotherapy or radiation.
- Stage III: Abnormal cells that have spread to your lymph nodes but not other organs. You will need surgery and chemotherapy and possibly radiation.
- Stage IV: Abnormal cells that have spread through your blood and lymph nodes to other organs. You will need surgery to remove them, if the cancerous area is not too large, and chemotherapy to shrink them or prolong life.
Updated:
May 15, 2023
Reviewed By:
Janet O'Dell, RN