Endometrial Cancer Symptoms
Abnormal bleeding is the warning sign that endometrial cancer cells may have begun to grow out of control in the inner lining of your uterus. Learn more here.
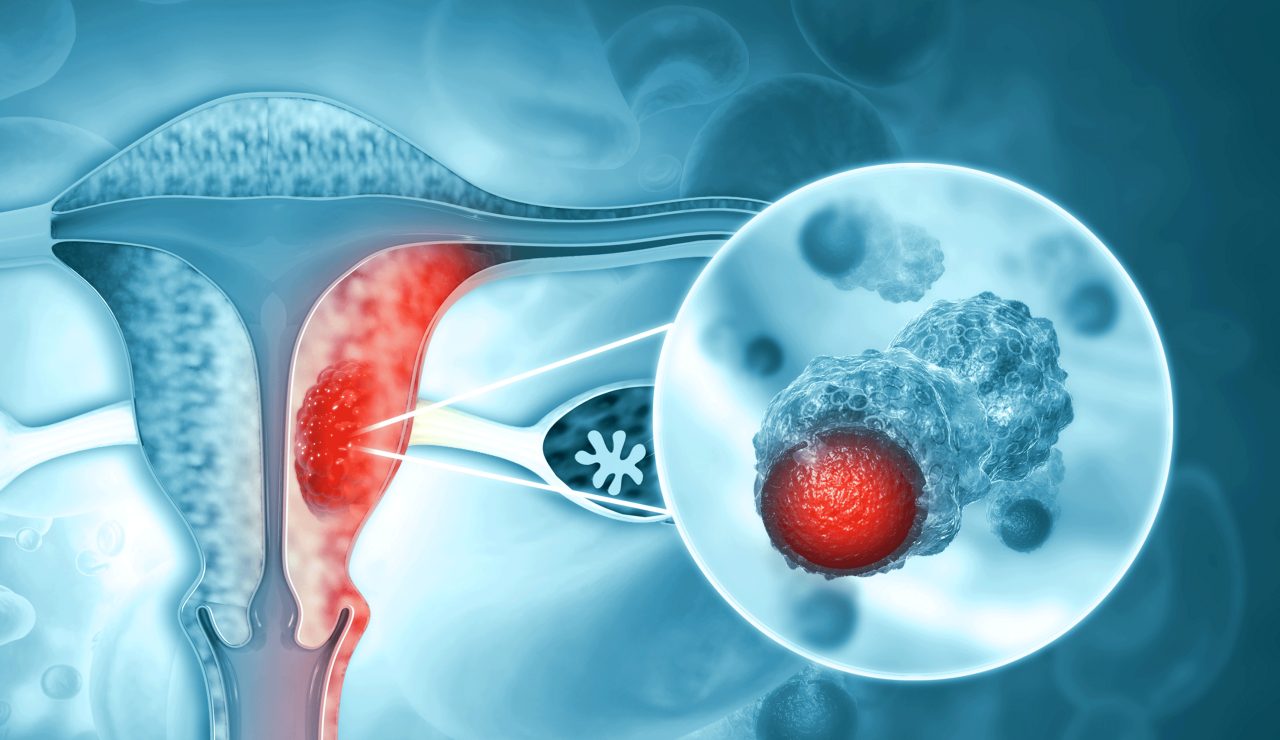
The uterus is a pear-shaped hollow in a woman’s pelvis, the space for a fetus to grow when a woman conceives. Its inner lining, the endometrium, sheds cells monthly during menstruation.
It’s possible for cells in that lining to begin growing out of control and become cancer. These cancer cells may eventually spread to the lymph nodes and elsewhere in your body.
According to the American Cancer Society, some 66,000 new U.S. cases of endometrial cancer will be diagnosed in 2022, with 12,550 women more likely to die of the disease. But more than 600,000 American women who have had endometrial cancer, sometimes called uterine cancer, are alive today.
YOU MIGHT ALSO LIKE: What Is Endometrial Cancer?
What are the signs and symptoms of endometrial cancer?
The tell-tale symptom is abnormal bleeding. You might have heavy bleeding in between periods, or you might bleed after menopause. Some women have an unusual watery, pink, or white discharge. Any discharge that smells bad is possibly a bad sign.
Don’t assume you have cancer. You may have a yeast infection or a different kind of infection, but get it checked out. See your gynecologist immediately even if you have only a little spotting after menopause.
Other symptoms include pelvic pain. You might have pain during sex. That said, many women have pelvic pain and pain during sex that is not caused by cancer.
Unexplained weight loss can be a symptom of endometrial cancer. Losing 10 or more pounds unintentionally may mean that your body is working hard to fight off tumor cells.
Unexplained fatigue is also worth evaluation. If your weeks haven’t been especially busy and you’ve had your usual amount of sleep, ongoing fatigue could be a sign that your body is fighting a tumor.
Frequent urination can be caused by a urinary tract infection. But if you don’t have an infection and you feel a special urgency to urinate, burning, bladder spasms, or difficulty emptying your bladder, it’s worth talking to your gynecologist further.
Your abdomen may stick out. You also might have symptoms associated with irritable bowel syndrome, such as diarrhea or constipation as well as bloating. Some women are used to gastrointestinal issues but end up being diagnosed during the later stages of endometrial cancer
Are your legs, ankles, or feet swollen or feel heavy? The skin may look stretched or shiny if you are retaining water, which can be an early sign of endometrial cancer.
Feeling full after a small meal can be an early sign. Some women become nauseated and vomit when they eat.
Some women have no symptoms at all.
It’s important to report any pain or bleeding (or two or more symptoms) to a gynecologist, even if you’ve already had a check-up that year with a pelvic exam and Pap smear. A PAP smear screens for early signs of cervical cancer, which is not the same as endometrial cancer. Pap smears can find some endometrial cancers early, but they are not a reliable screening method. A pelvic exam also isn’t likely to catch uterine cancer early, according to the American Cancer Society.
Testing for human papillomavirus, the common STD, also helps prevent cervical cancer, which the virus can cause, but it doesn’t screen for endometrial cancer.
How is endometrial cancer diagnosed?
If it appears that you may have this kind of cancer, your doctors will perform an endometrial biopsy. A thin flexible tube is inserted through your cervix into your uterus, where gentle scraping and suction remove a sample of tissue. That tissue can be examined under a microscope for signs of cancer cells.
In a hysteroscopy, your doctors will examine your uterus using a tube with a video camera at the tip and may also take a tissue sample.
In a dilation and curettage (or D&C), doctors widen your cervix to take a tissue sample.
How can you protect yourself against endometrial cancer?
The most important risk factor is obesity, so you can lose unnecessary weight to protect yourself. Using oral contraception may help as well. If you use hormone replacement therapy, take the lowest possible dose for the shortest period of time to minimize risk.
If family members have had colon cancer or endometrial cancer, you might visit a geneticist to see if you have a gene variant raising your risk for hereditary non-polyposis colon cancer (also known as HNPCC or Lynch syndrome), which increases your risk of endometrial cancer.
If you do have the gene, consider having a yearly endometrial biopsy beginning at age 35.
Updated:
January 03, 2023
Reviewed By:
Janet O'Dell, RN