What Is Pancreatitis?
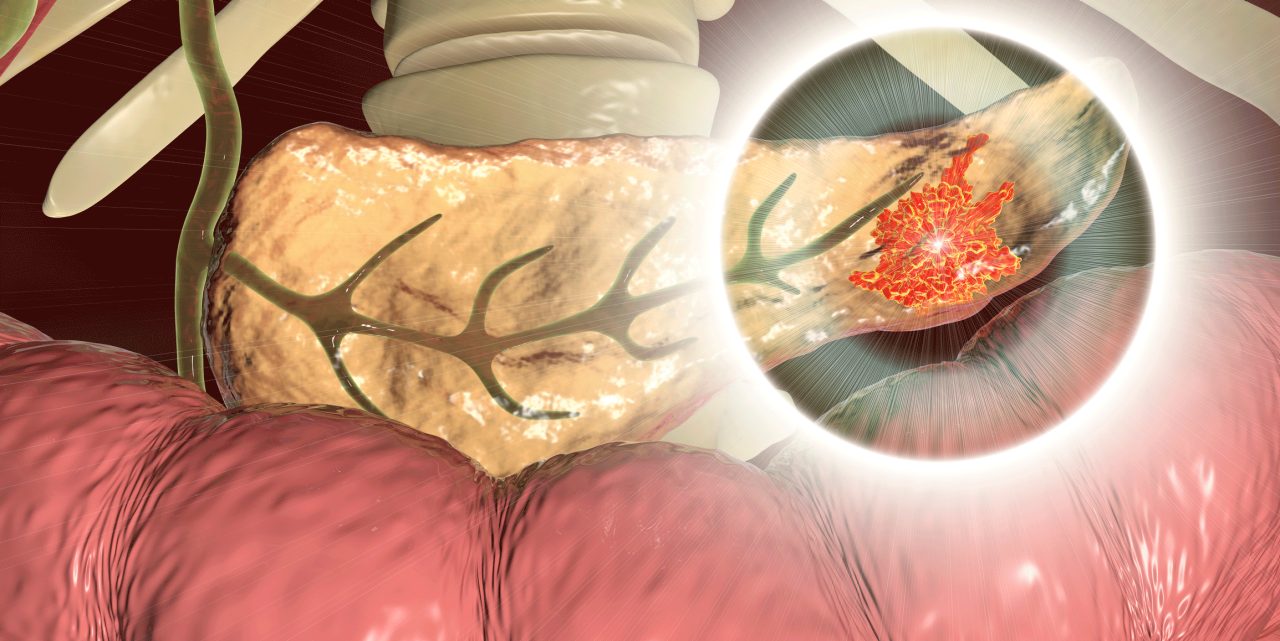
Pancreatitis occurs when your pancreas, which sits behind your stomach, becomes inflamed. Most people with pancreatitis feel some pain on their left side.
Do you have pain on the left side of your abdomen, nausea or vomiting, hiccups, and fever?
They could be signs of pancreatitis.
YOU MIGHT ALSO LIKE: Pancreatitis Symptoms
What is pancreatitis?
The pancreas sits behind your stomach, releasing enzymes that allow you to digest food. The pancreas also regulates how your body manages glucose, the problem with diabetes.
If it becomes inflamed, you have pancreatitis. Sometimes the problem comes and goes quickly, but it can also linger.
What are the symptoms of pancreatitis?
Most people who have acute or chronic pancreatitis feel some pain on their left side. It’s possible to have chronic pancreatitis that shows up on a scan, even though you haven’t had symptoms of pancreatitis.
Other possible signs include:
- Pain that wraps around your upper body and moves in bands on your back
- Indigestion
- Nausea or vomiting
- Abdominal tenderness
- Unintentional weight loss
- Bloating and a swollen abdomen
- Hiccups
- Fever
Unpleasant smelling stool (because your pancreas doesn’t supply enough digestive enzymes to break down your food)
What causes pancreatitis?
More than 3 million Americans have gallstones, hardened deposits of digestive fluid in your gallbladder that can trigger acute pancreatitis. The pain may come on very suddenly and require a hospital stay.
The first 24 hours after symptoms begin are a key time for doctors to determine whether you are at risk of serious complications.
The problem is more likely to become chronic if you smoke or drink alcohol. It can linger and produce scar tissue or keep coming back, damaging the cells that produce insulin. About 45 percent of people with chronic pancreatitis develop type 2 diabetes. Too much drinking causes more than two-thirds of chronic pancreatitis cases.
Cystic fibrosis and other illnesses can lead to chronic pancreatitis, so your doctors will have to explore your situation and rule out risks like pancreatic cancer.
Some people need to have their gallbladder, a small pear-shaped organ that you can spare, removed.
Pancreatitis can be serious. From 3 to 10 percent of patients die of acute pancreatitis. If you arrive at the hospital with a severe cause, your mortality risk jumps as high as 50 percent.
How is pancreatitis treated?
You may need to stay in the hospital and fast so your pancreas can rest, while you receive customized fluids and nutrition intravenously (IV). Once the inflammation subsides, you may begin receiving clear fluids and bland foods.
If pancreatitis persists, and you still feel pain after you eat, you may need a nasogastric feeding tube that goes from your nose directly into your stomach. In 65 to 85 percent of cases, the tube, along with medication for pain and perhaps artificial digestive enzymes, will help you recover.
Eventually, after a couple of days or up to two weeks, you can begin eating again. The remaining cases of pancreatitis are more serious because of risk factors like obesity or genetic vulnerability. You may need surgery to remove diseased parts of your pancreas.
Once you’re eating on your own, your diet will play a key role in your strategy to stay healthy. You’ll need to avoid:
- Red meat
- Fried food
- Full-fat dairy
- Sugary desserts and drinks
- Caffeine
- Alcohol
Favor smaller meals spread throughout the day, focusing on protein and vegetables. Make sure you stay hydrated.
Updated:
June 29, 2023
Reviewed By:
Janet O’Dell, RN