What Is a Pulmonary Embolism?
A pulmonary embolism is a life-threatening blockage in your lungs. Without a quick diagnosis and treatment, about one-third of people with the condition die.
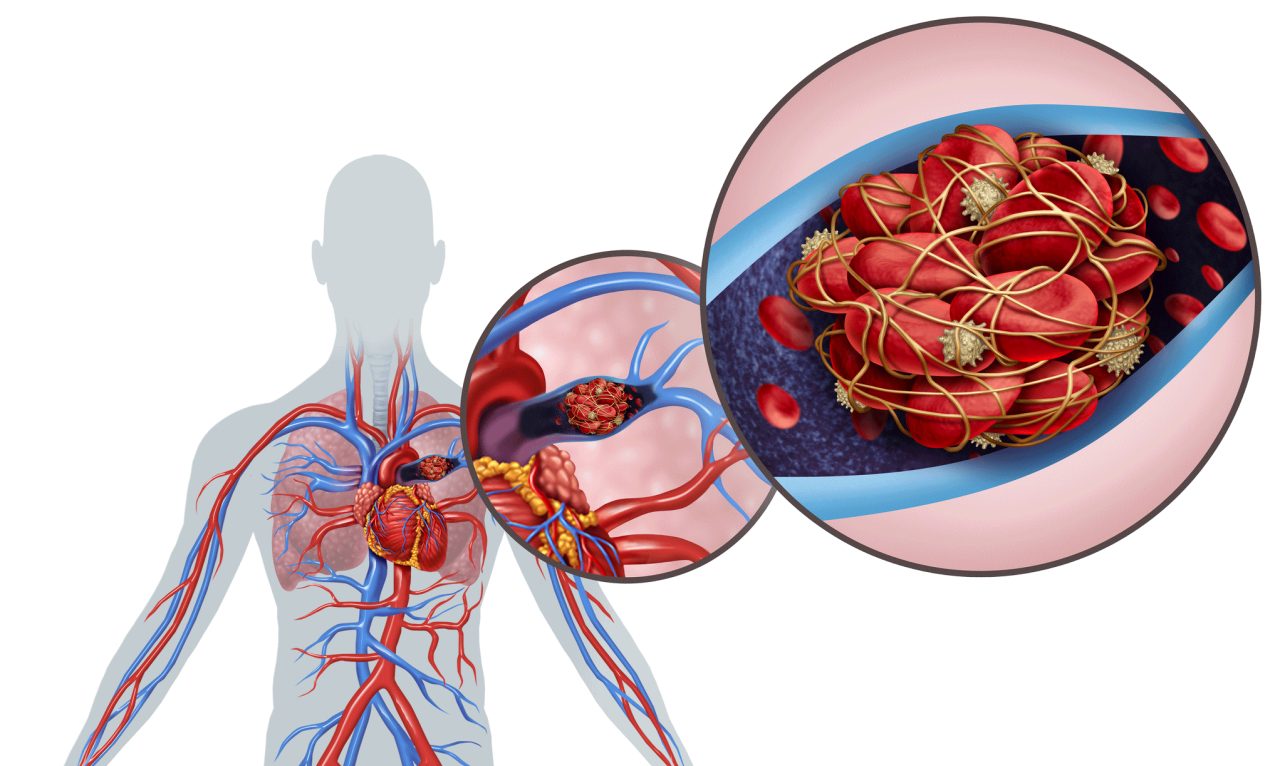
The clotting of blood is a natural and normal way your body heals damaged blood vessels — whether you’ve accidentally cut yourself or are recovering from surgery. But sometimes, blood clots can also cause serious illness. A pulmonary embolism (PE) is a case in point. In fact, ignoring risk factors and failing to act quickly to get help if you develop any PE symptoms can be deadly.
To understand what a pulmonary embolism is and why it is a potentially life-threatening condition, consider a blockage of arteries in your lungs can disrupt breathing and, in worst case scenarios, make it impossible to breathe.
A PE is usually the result of a blood clot that develops in a deep vein, most often in your lower leg, thigh, or pelvis. This deep vein thrombosis (DVT) can break off and travel through your bloodstream, all the way to your lungs, where it blocks an artery, causing a pulmonary embolism, the National Heart, Lung and Blood Institute (NHLB) explains.
Although rare, there are sometimes other causes of a pulmonary embolism — including fat from the marrow of a broken long bone or part of a tumor. These non-blood “clots” of material can become loose and flow with blood to your lungs.
YOU MIGHT ALSO LIKE: Signs and Symptoms of a Blood Clot
Look: Risk factors for pulmonary embolism
If you have to stay in bed to heal after surgery or an accident, or if you are in one position for a long time on a lengthy plane or car trip, the circulation of your blood slows because you stop moving as much as usual, raising the risk of a blood clot forming and moving to your lungs.
Other factors that can increase the risk of having a pulmonary embolism include your personal and family health history. For example, you are more likely to develop a PE if you or any first-degree relative have experienced a DVT or PE previously, the NHLBI points out. There are also some inherited disorders that can make blood more likely to clot.
Certain heart conditions, kidney disease, malignancies (especially cancers of the brain, pancreas, stomach, kidneys, and lungs), and chemotherapy increase the risk, too.
Pregnancy can cause blood clots that can become pulmonary embolisms in two ways. If you are placed on bed rest due to pregnancy complications, being immobile raises your risk. In some women, the weight of their unborn baby presses on veins in their pelvis area, slowing down blood flow from the legs, making blood clots more likely to form.
Smoking and being overweight are also linked to more incidents of pulmonary embolisms, especially if you have additional risk factors.
We can’t emphasize this enough: Pulmonary embolism symptoms need urgent care
Unfortunately, about one in four people with a pulmonary embolism dies without any warning signs, according to the Centers for Disease Control and Prevention (CDC). That’s why it’s important to work with your doctor to lower any risk factors you have for PEs and to take anti-coagulant medications if prescribed.
Signs of a pulmonary embolism can vary a great deal, depending on the size and number of clots, how much of your lung is affected, and whether you have another heart or lung disease.
Here are the most common symptoms:
- Feeling short of breath. Usually the breathlessness is sudden and worsens with physical exertion.
- Coughing. Coughing up bloody sputum often occurs with a PE.
- Chest pain. This may be mistaken for a heart attack and is often sharp, especially when you take a deep breath.
Less common symptoms associated with pulmonary embolisms include feeling dizzy, very low blood pressure, an irregular or faster than normal heartbeat, excessive perspiration and, sometimes, fever.
Any signs of a pulmonary embolism should signal getting immediate, urgent medical care, according to the CDC.
A severe, life-threatening pulmonary embolism, if caught in time, can be treated with thrombolytics, medications that dissolve blood clots. Your doctor may prescribe other anticoagulants to prevent additional clots from forming in the future; some people may need to take these drugs regularly, long-term, to prevent future blood clots and PEs.
Updated:
October 14, 2020
Reviewed By:
Janet O’Dell, RN