When Your Child Has an Object in the Ear or Nose
When Your Child Has an Object in the Ear or Nose
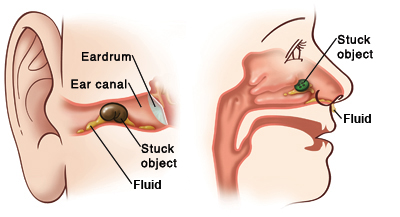
Children often put small objects such as food or toys in their ears or nose. If these objects get stuck, fluid can build up in the ear or nose. This can cause an infection.
An object put in the nose can even be inhaled into the lungs. An object in the ear may put a hole in (puncture) the eardrum or cause hearing loss. An object can also harm body tissue and may be hard to remove.
Symptoms of blockage in the ear or nose
Your child may have an object stuck in an ear if he or she has any of the following:
-
Pain in the ear
-
Fluid draining from the ear
-
Hearing loss
-
Irritation. The child may pick at or play with the ear.
Your child may have something stuck in the nose if he or she has any of the following:
-
Bad smelling, yellowish, or bloody fluid draining from the nose
-
Blocked breathing from one side of the nose
A blockage sometimes causes no symptoms at all.
Keep small batteries away from small children. These batteries include those used in watches, cameras, and hearing aids. These button-like batteries can easily get stuck in the ear or nose. If they become stuck, acid from the battery can leak out and burn the inside of the ear or nose. So be sure to store these batteries properly. When they are no longer needed, throw them away properly.
If an object is stuck in an ear or nose:
-
Don't try to remove the object. This can push the object in farther and make it harder to remove.
-
Don’t use a cotton swab to remove the object. You will only push the object in farther.
-
Don’t pour anything into the ear or nose.
Trying to remove the object without the proper tools can also make your child’s ear or nose sore and painful. This will make your child less likely to cooperate when the healthcare provider later tries to remove the object.
Instead, call your child’s healthcare provider or go to the emergency room. The provider may have you bring the child to the office or refer you to an ENT doctor (otolaryngologist). An ENT doctor has the tools needed to remove the object.
What the healthcare will do
The doctor will remove the object using the proper tools. If your child is fussing and can’t stay still, the doctor may need to swaddle or gently restrain your child to prevent damaging the ear or nose. If your child can't stay calm, he or she may need general anesthesia. This is medicine that allows your child to sleep. If anesthesia is used, your child will be taken to the operating room to have the object removed. Once the object is removed, the doctor may prescribe medicines or ointment to prevent infection. Use the medicine on your child as directed. And call the doctor if you see any signs of infection such as fever (see Fever and children, below) or soreness of the ear or nose.
Preventing future blockages
To help prevent objects from getting stuck in your child’s ear or nose:
-
Keep small objects away from children.
-
Avoid using cotton swabs to clean your child’s ear canals. They tend to push in wax and can harm the eardrum. Instead, use a washcloth wet with warm water and soap. Then rinse and wipe the ear with a towel.
Fever and children
Always use a digital thermometer to check your child’s temperature. Never use a mercury thermometer.
For infants and toddlers, be sure to use a rectal thermometer correctly. A rectal thermometer may accidentally poke a hole in (perforate) the rectum. It may also pass on germs from the stool. Always follow the product maker’s directions for proper use. If you don’t feel comfortable taking a rectal temperature, use another method. When you talk to your child’s healthcare provider, tell him or her which method you used to take your child’s temperature.
Here are guidelines for fever temperature. Ear temperatures aren’t accurate before 6 months of age. Don’t take an oral temperature until your child is at least 4 years old.
Infant under 3 months old:
-
Ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead (temporal artery) temperature of 100.4°F (38°C) or higher, or as directed by the provider
-
Armpit temperature of 99°F (37.2°C) or higher, or as directed by the provider
Child age 3 to 36 months:
-
Rectal, forehead (temporal artery), or ear temperature of 102°F (38.9°C) or higher, or as directed by the provider
-
Armpit temperature of 101°F (38.3°C) or higher, or as directed by the provider
Child of any age:
-
Repeated temperature of 104°F (40°C) or higher, or as directed by the provider
-
Fever that lasts more than 24 hours in a child under 2 years old. Or a fever that lasts for 3 days in a child 2 years or older.
Updated:
March 16, 2019
Sources:
Foreign Bodies in the Ear, Nose, and Throat. Heim SW. American Family Physician. 2007;87(8):1185-9.
Reviewed By:
Ashutosh Kacker MD