Myasthenia Gravis
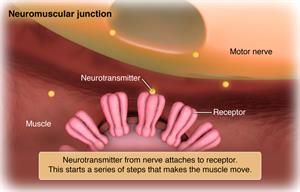
Myasthenia gravis is a chronic, complex, autoimmune disorder in which the body attacks its own neuromuscular connections. This causes problems with communication between nerves and muscle, resulting in weakness. Myasthenia gravis affects the voluntary muscles of the body, especially the eyes, mouth, throat, and limbs.
In women, myasthenia gravis generally starts by age 20 to 30. In men, it usually starts after the age of 50. However, this condition can occur at any age. Males are more often affected than females.
Myasthenia gravis is not inherited and it is not contagious. It generally develops later in life when antibodies in the body attack normal receptors on muscle. This blocks a chemical needed to stimulate muscle contraction.
A temporary form of myasthenia gravis may develop in the fetus when a woman with myasthenia gravis passes the antibodies to the fetus. Generally, it resolves in 2 to 3 months.
These are the most common symptoms of myasthenia gravis:
- Visual problems, including drooping eyelids (ptosis) and double vision (diplopia)
- Muscle weakness and fatigue may vary rapidly in intensity over days or even hours and worsen as muscles are used (early fatigue)
- Facial muscle involvement causing a mask-like appearance; a smile may appear more like a snarl
- Trouble swallowing or pronouncing words
- Weakness of the neck or limbs
The symptoms of myasthenia gravis may look like other conditions. Always see your doctor for a diagnosis.
Flare-ups and remissions (easing of symptoms) may occur now and then during the course of myasthenia gravis. Remissions, however, are only rarely permanent or complete.
Your doctor can diagnose myasthenia gravis based on your symptoms and certain tests. During the physical exam, your doctor will ask about your medical history and symptoms.
A common way to diagnose myasthenia gravis is to test how you respond to certain medicines. Muscle weakness often dramatically improves for a brief time when you are given an anticholinesterase medicine. If you respond to the medicine, it confirms myasthenia gravis.
Other tests that may be done include:
- Blood tests. These tests look for antibodies that may be present in people with myasthenia gravis.
- Genetic tests. These tests are done to check for conditions that run in families.
- Nerve conduction studies. A test called repetitive nerve stimulation is used to diagnose myasthenia gravis.
- Electromyogram (EMG). A test that measures the electrical activity of a muscle. An EMG can detect abnormal electrical muscle activity due to diseases and neuromuscular conditions.
Specific treatment for myasthenia gravis will be determined by your healthcare provider based on:
- How old you are
- Your overall health and medical history
- How sick you are
- How well you can handle specific medicines, procedures, or therapies
- How long the condition is expected to last
- Your opinion or preference
There is no cure for myasthenia gravis, but the symptoms can often be controlled. Myasthenia gravis is a lifelong medical condition. Early detection is the key to managing the condition.
The goal of treatment is to increase muscle function and prevent swallowing and breathing problems. Most people with this condition can improve their muscle strength and lead normal or near normal lives. In more severe cases, help may be needed for breathing and eating.
Treatment may include:
- Medicine. Anticholinesterase medicines, steroids, or medicines that suppress the immune system’s response (immunosuppressive) medicines may be used.
- Thymectomy. This is surgical removal of the thymus gland. The role of the thymus gland in myasthenia gravis is not fully understood, and the thymectomy may or may not improve symptoms. However, it reduces symptoms in more than 70% of people who do not have cancer of the thymus, possibly by altering the immune system response.
- Plasmapheresis. A procedure that removes abnormal antibodies from the blood and replaces the blood with normal antibodies from donated blood.
- Immunoglobulin. A blood product that helps decrease the immune system’s attack on the nervous system. It is given intravenously (IV).
The most serious complications of myasthenia gravis is a myasthenia crisis. This is a condition of extreme muscle weakness, particularly of the diaphragm and chest muscles that support breathing. Breathing may become shallow or ineffective. The airway may become blocked because of weakened throat muscles and build up of secretions. Myasthenia crisis may be caused by a lack of medicine or by other factors, such as a respiratory infection, emotional stress, surgery, or some other type of stress. In severe crisis, a person may have to be placed on a ventilator to help with breathing until muscle strength returns with treatment.
Precautions, which may help to prevent or minimize the occurrence of myasthenia crisis include:
- Taking anticholinesterase medicines 30 to 45 minutes before meals to reduce the risk of aspiration (food entering the lung passages)
- Taking anticholinesterase medicines exactly as prescribed to help maintain the strength of the breathing muscles
- Avoiding crowds and contact with people with respiratory infections, such as a cold or the flu
- Taking in proper nutrition to maintain optimal weight and muscle strength
- Balancing periods of physical activity with periods of rest
- Using stress-reduction techniques and avoiding emotional extremes
Tell your healthcare providers about your condition when any medicines are being prescribed. Certain medicines may interfere either with the disease or the action of the medicines you take for myasthenia gravis.
There is no cure for myasthenia gravis, but the symptoms can generally be controlled. Myasthenia gravis is a lifelong medical condition. Early detection is key to managing this condition.
The goal of treatment is to increase general muscle function and prevent swallowing and breathing problems. Most people with myasthenia gravis can improve their muscle strength and lead normal or near normal lives. In more severe cases, help may be needed with breathing and eating.
Call your doctor if any of these occur:
- Drooping eyelid
- Blurred or double vision
- Slurred speech
- Problems chewing and swallowing
- Weakness in the arms and legs
- Chronic fatigue
- Trouble breathing
- Myasthenia gravis is a chronic, complex, autoimmune disorder in which antibodies destroy neuromuscular connections. This causes problems with communication between nerves and muscle, resulting in weakness of the skeletal muscles. It affects the voluntary muscles of the body, especially the eyes, mouth, throat, and limbs.
- There is no cure for myasthenia gravis, but the symptoms can generally be controlled.
- The goal of treatment is to increase general muscle function and prevent swallowing and breathing problems.
- Most people with this condition can improve their muscle strength and lead normal or near normal lives.
- In more severe cases, help may be needed for breathing and eating.
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Updated:
January 16, 2018
Reviewed By:
Shelat, Amit, MD,Dozier, Tennille, RN, BSN, RDMS